Understanding Teeth Whitening Sensitivity
Teeth whitening is a popular cosmetic procedure, sought after by many to enhance their smiles. However, a common concern among those considering or undergoing whitening treatments is the potential for increased tooth sensitivity. This sensitivity can range from mild discomfort to sharp, sudden pain, triggered by hot or cold foods and drinks, or even air. Understanding the underlying causes and management strategies for this sensitivity is crucial for anyone looking to brighten their teeth. It’s important to differentiate between temporary and potentially long-lasting sensitivity, as well as to consider individual factors that can influence the experience. This article will delve into the various aspects of teeth whitening sensitivity, providing a comprehensive guide to help you navigate this process safely and effectively. The goal is to empower you with the knowledge to make informed decisions and maintain optimal oral health.
What Causes Sensitivity After Whitening?
The primary culprit behind sensitivity after teeth whitening is the bleaching agent, typically hydrogen peroxide or carbamide peroxide. These agents work by penetrating the enamel to break down stains and discoloration. This process, while effective, can also irritate the nerves within the teeth, leading to heightened sensitivity. Several factors contribute to how intensely an individual experiences this sensitivity. The concentration of the whitening agent, the duration of its contact with the teeth, and the frequency of treatments all play a role. In addition, individual differences in tooth structure and existing dental conditions can significantly impact the level of sensitivity experienced. Being aware of these underlying mechanisms is the first step in managing and minimizing discomfort during and after teeth whitening procedures. Addressing these causes can improve the whitening experience and support ongoing oral health.
The Role of Whitening Agents
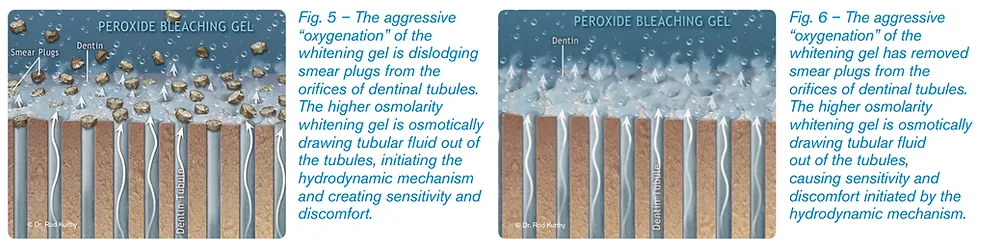
Whitening agents, predominantly hydrogen peroxide and carbamide peroxide, are the workhorses of teeth whitening. Hydrogen peroxide, in varying concentrations, is a direct bleaching agent, while carbamide peroxide breaks down into hydrogen peroxide. These compounds effectively lift stains from the enamel, leading to a brighter smile. However, this process isn’t without its side effects. As the whitening agents penetrate the enamel, they can also pass through to the dentin, the layer beneath the enamel, which contains tiny tubules leading to the tooth’s nerve. This interaction with the nerve endings is what causes the sensitivity. The higher the concentration of the whitening agent, the greater the potential for sensitivity. Professional treatments, which use higher concentrations, may lead to more pronounced sensitivity compared to over-the-counter options.
Enamel Thinning & Sensitivity
Enamel is the hard, protective outer layer of the tooth. Its thickness and integrity are crucial in preventing sensitivity. Whitening agents, while effective, can slightly dehydrate the enamel, making it more porous. This increased porosity allows for easier access of external stimuli, such as hot or cold substances, to the underlying nerves. Additionally, repeated whitening treatments or the use of abrasive whitening products can contribute to the erosion of enamel over time. This thinning of the enamel exposes the dentin and nerves, intensifying sensitivity. Maintaining enamel health is therefore essential when undergoing teeth whitening. This includes using gentle brushing techniques, avoiding highly acidic foods and drinks, and considering enamel-strengthening treatments recommended by a dentist.
Gum Recession & Sensitivity
Gum recession, where the gum tissue pulls back, exposing more of the tooth’s root, is another contributing factor to teeth sensitivity. The roots of the teeth are not covered by enamel, making them naturally more sensitive. When gums recede, these sensitive root surfaces become exposed to the whitening agents and external stimuli. Individuals with gum recession may experience heightened sensitivity during teeth whitening procedures. Addressing gum health is crucial to mitigate this issue. Regular dental checkups, proper brushing techniques, and sometimes professional treatments to address gum recession can help minimize discomfort. If you have concerns about gum recession, consulting with a dentist before undergoing teeth whitening is advisable.
Top 5 Factors Influencing Sensitivity

- Whitening Method: Professional treatments vs. at-home kits.
- Tooth Sensitivity Threshold: Individual differences in nerve sensitivity.
- Oral Hygiene Practices: Brushing and flossing habits.
- Pre-existing Dental Conditions: Cavities, cracks, or gum disease.
- Whitening Agent Concentration: Higher concentrations often lead to more sensitivity.
How Long Does Whitening Sensitivity Last?
The duration of sensitivity after teeth whitening can vary greatly from person to person. In most cases, the sensitivity is temporary, subsiding within a few days to a couple of weeks after the whitening treatment is completed. However, in some instances, the sensitivity may linger for a longer period, potentially several months, especially if the teeth are already prone to sensitivity or if the whitening procedure was aggressive. The intensity of the sensitivity also plays a role; mild discomfort tends to resolve quicker than more severe pain. Understanding the expected timeframe and potential factors that influence the duration of sensitivity is crucial to manage expectations and address concerns effectively.
Managing Short-Term Sensitivity
Managing short-term sensitivity involves several strategies aimed at soothing the nerves and reducing discomfort. One of the simplest and most effective methods is to avoid extremely hot or cold foods and drinks. Switching to lukewarm or room-temperature options can significantly minimize triggering pain. Additionally, using a desensitizing toothpaste that contains ingredients like potassium nitrate can provide relief. These toothpastes work by blocking the tubules in the dentin, thus reducing nerve sensitivity. Over-the-counter pain relievers, such as ibuprofen, can also be helpful in managing any discomfort. If the sensitivity is severe, a dentist might recommend a fluoride treatment to strengthen the enamel and reduce nerve exposure.
Desensitizing Toothpaste

Desensitizing toothpastes are specifically formulated to combat tooth sensitivity. They contain active ingredients, such as potassium nitrate or stannous fluoride, that help block the pain signals from reaching the nerve. Potassium nitrate works by penetrating the tooth and calming the nerve, while stannous fluoride helps to block the tubules and protect the enamel. To get the best results, it’s generally recommended to brush with desensitizing toothpaste twice a day, using a soft-bristled toothbrush. It may take several weeks of consistent use to notice significant improvements in sensitivity. Consider consulting with a dentist to choose the best desensitizing toothpaste for your specific needs.
Fluoride Treatments
Fluoride treatments are a valuable tool in managing tooth sensitivity after whitening. Fluoride strengthens the enamel, making it more resistant to acid attacks and reducing the permeability of the enamel. This, in turn, helps to minimize sensitivity by creating a protective barrier over the exposed dentin. Professional fluoride treatments administered by a dentist provide a higher concentration of fluoride, offering more immediate relief. These treatments can be in the form of fluoride varnish, gels, or foams. Fluoride can also be obtained through prescription toothpaste or mouth rinses. Regular fluoride use, along with good oral hygiene practices, can significantly reduce sensitivity and promote overall oral health.
Dietary Adjustments
Making dietary adjustments can play a significant role in managing sensitivity after teeth whitening. Avoiding highly acidic foods and beverages, such as citrus fruits, sodas, and vinegar-based dressings, can help prevent further enamel erosion and irritation. These acids can dissolve the minerals in the enamel, making the teeth more vulnerable to sensitivity. It’s also advisable to reduce the consumption of extremely hot or cold items, as these can trigger discomfort. Focusing on a balanced diet rich in calcium and other nutrients essential for healthy teeth and gums is recommended. Drinking plenty of water helps maintain hydration and promotes saliva production, which neutralizes acids and remineralizes the enamel. These dietary adjustments can contribute to a smoother and more comfortable post-whitening experience.
When to Consult a Dentist

While some sensitivity after teeth whitening is normal, it’s crucial to know when to seek professional dental advice. If the sensitivity is severe, persistent, or worsening despite home remedies, it is essential to consult a dentist. Other concerning symptoms include sharp, shooting pains, throbbing, or discomfort that lingers for more than a few weeks. These symptoms may indicate an underlying dental issue that needs to be addressed. Additionally, if you experience any changes in your gums, such as redness, swelling, or bleeding, a dentist should be consulted promptly. A dentist can assess the situation, identify the cause of the sensitivity, and recommend appropriate treatments, such as fluoride treatments, desensitizing agents, or other interventions to alleviate the discomfort and address any underlying dental problems.
Persistent Sensitivity Symptoms
Persistent sensitivity symptoms require immediate attention from a dentist. If the sensitivity does not improve or worsens after several weeks, it could be a sign of a more serious issue. Severe, sharp pain, throbbing sensations, or pain that interferes with daily activities warrant an evaluation. Moreover, if the sensitivity is accompanied by other symptoms, such as pain when biting or chewing, swelling, or redness of the gums, a dental visit is necessary. The dentist can perform a thorough examination, taking X-rays if needed, to identify the root cause of the sensitivity. Early diagnosis and treatment can prevent the problem from worsening and help to ensure long-term oral health.
Possible Underlying Dental Issues
Persistent sensitivity after teeth whitening may indicate underlying dental issues. Cavities, cracks in the teeth, and gum disease can all contribute to heightened sensitivity. These conditions expose the dentin or the tooth’s nerve, making them more vulnerable to stimuli. If your dentist identifies any of these issues, they will recommend appropriate treatments. For cavities, fillings may be necessary. Cracks in the teeth may require bonding or crowns. Gum disease needs professional treatment and improved oral hygiene practices. Addressing these underlying issues is crucial, not only to alleviate sensitivity but also to preserve your overall oral health. A comprehensive dental examination is vital to identify and treat any contributing factors to teeth sensitivity.
Long-Term Solutions for Sensitive Teeth

Long-term solutions for managing sensitive teeth often involve a combination of professional treatments and at-home care. Your dentist may recommend fluoride treatments to strengthen the enamel and reduce sensitivity. Dental bonding can be used to protect exposed root surfaces or repair minor enamel defects. In more severe cases, treatments like root canals may be necessary to address nerve damage. Maintaining excellent oral hygiene practices is crucial for long-term oral health. This includes regular brushing with a soft-bristled toothbrush, flossing daily, and using a desensitizing toothpaste. Routine dental checkups and professional cleanings are also essential for identifying and addressing any underlying issues. Consistent care and adherence to your dentist’s recommendations can contribute to a healthier, less sensitive smile.
Preventative Measures to Reduce Sensitivity
Several preventative measures can be taken to reduce the likelihood of experiencing sensitivity after teeth whitening. Choosing the right whitening products is important. Consider over-the-counter products with lower concentrations of whitening agents or consult with a dentist about professional options. Following all instructions carefully is important to minimize the risk of sensitivity. Practicing good oral hygiene is another key. This includes brushing gently with a soft-bristled toothbrush, flossing daily, and using a desensitizing toothpaste before and after whitening treatments. Avoiding abrasive whitening products, such as those containing harsh chemicals, can also help protect your enamel. Furthermore, maintaining a balanced diet and avoiding excessive consumption of acidic foods and beverages helps maintain enamel strength. These preventative measures can significantly reduce the chances of experiencing post-whitening sensitivity.
Choosing the Right Whitening Products
Selecting the right whitening products is crucial to minimize sensitivity and achieve the desired results. Over-the-counter products come in various forms, including strips, gels, and toothpastes, with varying concentrations of whitening agents. If you are prone to sensitivity, consider options with lower concentrations or those designed for sensitive teeth. For professional whitening, discuss your concerns with your dentist, who can recommend customized treatments. They can use desensitizing agents before and after the procedure to help minimize discomfort. Always follow the product instructions carefully. Avoid using products with harsh abrasives, which can damage enamel. Consider products that contain ingredients like potassium nitrate or fluoride. These can help to reduce sensitivity and protect your teeth.
Maintaining a Healthy Oral Routine

Maintaining a healthy oral routine is fundamental to minimizing sensitivity and achieving optimal oral health. This routine includes brushing your teeth twice a day for two minutes, using a soft-bristled toothbrush and fluoride toothpaste. Brushing gently, applying only moderate pressure, is important to avoid damaging the enamel. Flossing daily is equally important to remove plaque and food particles from between the teeth and along the gum line. This also helps prevent gum recession, which can contribute to sensitivity. Regular dental checkups and professional cleanings are vital for detecting and addressing any issues early on. Following a balanced diet, drinking plenty of water, and avoiding excessive consumption of sugary and acidic foods will further support your oral health. A consistent and comprehensive oral hygiene routine is your best defense against tooth sensitivity and other dental problems.
Conclusion
Experiencing sensitivity after teeth whitening is a common phenomenon, but it’s rarely permanent. Understanding the causes, factors, and management strategies can empower you to achieve a brighter smile while minimizing discomfort. The key lies in choosing the right whitening method, practicing good oral hygiene, and being proactive in addressing any sensitivity issues. Remember to consult with your dentist if you have any concerns or if the sensitivity persists. With the right approach, you can enjoy the benefits of teeth whitening without compromising your oral health and comfort. By following the guidelines in this article, you can make informed decisions and maintain a healthy and radiant smile. Prioritizing your oral health is an investment that pays dividends for years to come.
